Kidney diseases are very common in rabbits, and many remain undiagnosed. Healthy rabbits, when fed fresh food, rarely drink. If your rabbit is drinking a lot, it is almost always a sign of an underlying illness.
Contents
Symptoms: Recognizing Kidney Disease

Symptoms of Acute Renal Insufficiency:
- Altered general condition, apathy
- Fatigue
- Reduced or complete loss of appetite
- In the final stage: seizures and neurological symptoms
Symptoms of Chronic Renal Insufficiency:
Rabbits can live for years with chronic renal insufficiency without showing symptoms. Therefore, blood checks are important.
- Drinking (healthy rabbits fed fresh food drink almost nothing; drinking may be a sign of illness!)
- Altered general condition, apathy
- Gradual or significant weight loss, weight loss
- Increased urination (clear, absolutely transparent), incontinence
- Dull, unkempt, or scruffy fur
- Dehydration (skin fold does not return)
- Pale mucous membranes
- Reduced or complete loss of appetite, picky eating behavior (often leading to tooth spikes)
- Bladder grit due to impaired kidney function
Causes
Causes of Acute Renal Insufficiency:
- Bacteria (e.g. untreated bladder infections)
- Acute poisoning or prolonged use of medications (painkillers!)
- Digestive disorders, especially intestinal obstruction
- Chronic pain and stress conditions
- Obstruction of the ureters
Causes of Chronic Renal Insufficiency:
- Kidney stones / kidney grit (Nephrolithiasis)
- The pathogen E. Cuniculi
- Benign and malignant tumors of the kidney (e.g. renal carcinoma, leukemia)
- Kidney cysts
- Lack of water supply and dry feeding
- Bladder grit and stones (Urolithiasis, which can lead to backflow into the kidneys)

Diagnosis
Diagnostics in Acute Renal Insufficiency:
- Blood: Drastic increase in kidney values (creatinine, sometimes urea), inflammation markers (leukocytosis, pseudoleukocyte shift).
- Urine: Normal or clear (with low pH), possibly somewhat slimy. Often, leukocytes, erythrocytes, and epithelial cells can be detected. Sodium is decreased, and potassium is elevated. A bacteriological examination with antibiogram is recommended: The best sample is urine obtained via bladder puncture, as spontaneous urine is unsuitable, and catheterized urine is also less ideal due to possible contamination during urine collection.
Diagnostics in Chronic Renal Insufficiency
- Palpation: Possibly enlarged or shrunk and painful kidneys.
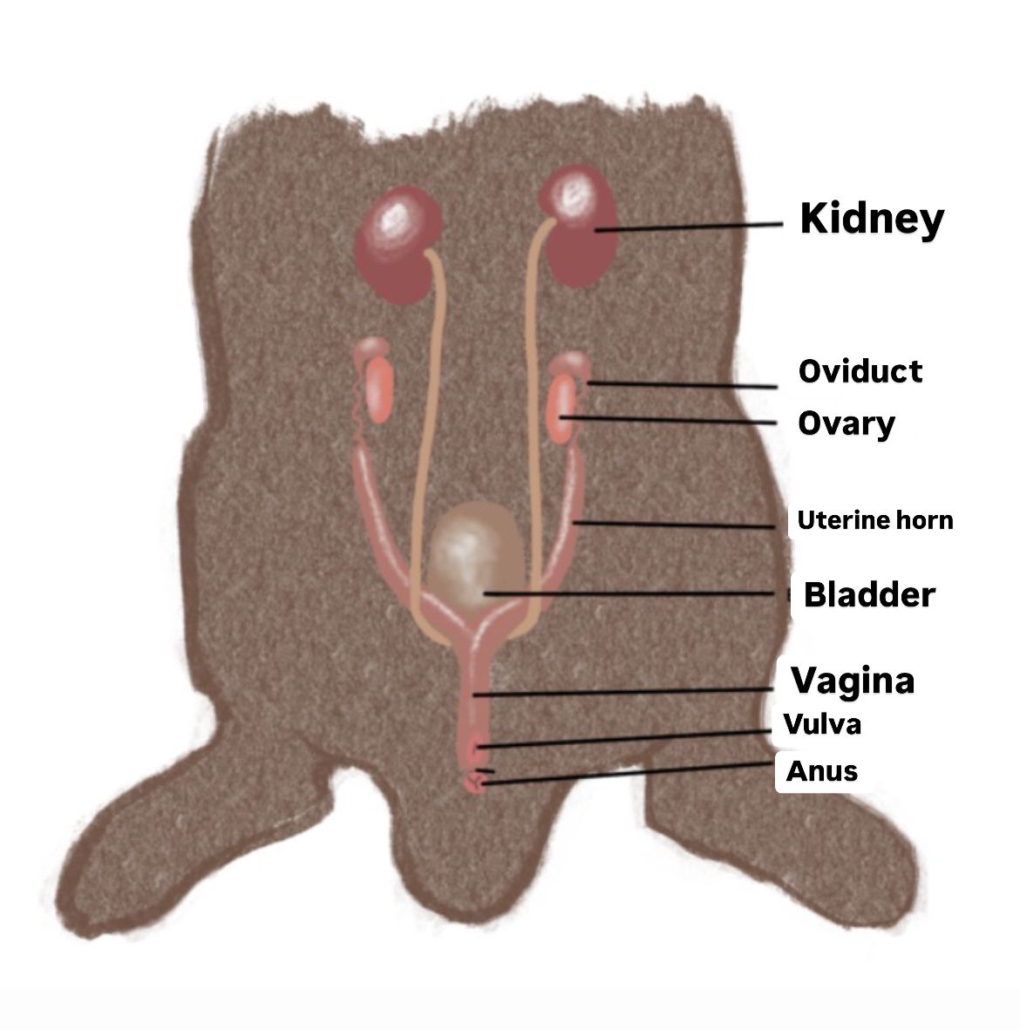
- X-ray or Ultrasound (to rule out kidney stones): Structural changes in kidney tissue are visible on ultrasound, enlarged kidneys in cases of kidney stones, and smaller kidneys in cases of E. Cuniculi. Demineralization in the bones may be visible on X-ray.
- Urine: Urine status and sediment findings in renal insufficiency: Very clear urine, lowered pH (Normal: 8-9), increased protein content. In severe renal insufficiency, ketones and glucose may also be detectable. Epithelial cells can also be found.
- Blood: Elevated creatinine and urea levels, with urea being significantly influenced by other factors. In the course of the disease, non-regenerative anemia and electrolyte shifts (hyperkalemia, hyponatremia) can occur. Secondary inflammations may also arise (pseudoleukocyte shift, leukocytosis), and liver values may increase as a result. It is important to request both EC titers (IgM and IgG) when diagnosing renal insufficiency
Treatment
Acute Renal Insufficiency
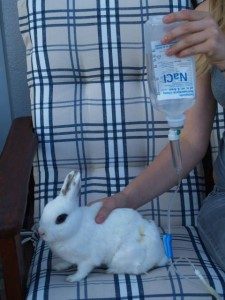
- Infusions: Full electrolyte solution (Ringer’s Lactate, Sterofundin), or NaCl if sodium is very low and potassium is too high. Administer 80-100 ml/kg intravenously once a day, or 40 ml/kg subcutaneously twice a day, with the possibility of decreasing frequency once stable. Infusion equipment and yellow cannulas (20G) or butterfly needles are needed.
- Broad-spectrum antibiotics (e.g., Marbofloxacin), possibly adjusted according to the results of the antibiogram.
- Forced feeding in case of refusal to eat.
- Pure fresh feeding.
- Liver supplements (for liver damage), such as milk thistle seeds (see link!).
- Possibly Zylexis.
- MCP (e.g., Emeprid) for nausea (which causes poor eating), and if given for more than 3 days, slowly taper off.
- SUC (S = Solidago compositum ad us. vet., U = Ubichinon compositum, C = Coenzyme compositum ad us. vet., homeopathic from Heel), 0.5 ml of each component subcutaneously or orally twice a day as a cure or long-term treatment. The effect of homeopathic remedies is not scientifically proven.
Chronic Renal Insufficiency
- Infusions: Full electrolyte solution (Ringer’s Lactate, Sterofundin), or NaCl if sodium is very low and potassium is too high.Administer 80–100 ml/kg intravenously once a day, or 40 ml/kg subcutaneously twice a day, with the possibility of less frequent administration once stable. Infusion equipment and yellow cannulas (20G) or butterfly needles are required.
- The determination of the UPC ratio is a simple method used to measure how much protein is being lost through the kidneys (reference range 0.11-0.4). To reduce these losses, ACE inhibitors (e.g., Benazepril Fortekor) or Angiotensin-II receptor blockers (e.g., Telmisartan – Semintra) are used.
- Possibly supplemental feeding in case of refusal to eat.
- MCP (e.g., Emeprid) for nausea (which causes poor eating), and if given for more than 3 days, should be slowly tapered off.
- Pure fresh feeding.
- Possibly Panacur (if E. Cuniculi is the cause).
- Possibly kidney surgery (if kidney stones or kidney tumors are the cause), only possible if the other kidney is functioning well (ultrasound, blood tests, and excretory urography, kidney scintigraphy (CT/MRI)). Nephrectomy (removal of a kidney, especially when multiple small stones or severe damage are present) or Nephrotomy (removal of the stone while preserving the kidney) is possible.
- Possibly treatment of bladder grit.
- Possibly pain relief for kidney stones.
- Liver supplements (for liver damage), e.g., milk thistle seeds.
- SUC (S = Solidago compositum ad us. vet., U = Ubichinon compositum, C = Coenzyme compositum ad us. vet., homeopathic from Heel) 0.5 ml of each component subcutaneously or orally twice a day as a cure or for long-term use. The effectiveness of homeopathic remedies is not scientifically proven.
If the condition is recognized and treated early, the progression of the disease can be halted and the animals can be stabilized, allowing them to live with it for some time. However, renal insufficiency cannot be cured. Affected rabbits need to be treated permanently.
Determining infusion volumes
Maintenance requirement: 50 ml/kg body weight/day
Deficit: Plus 50 ml/kg/day in case of loss (e.g., due to diarrhea)
Never give more than 40 ml/kg subcutaneously at once.
Determine the deficit:
| Dehydration Status | Clinical Symptoms | Infusion Volume |
| 5-6% | Slightly delayed skin fold return | Maintenance requirement 50ml/kg + 50-60ml deficit |
| 6-8% | Sticky mucous membranes, clearly delayed return of the skin fold | Maintenance requirement 50ml/kg + 60-80ml deficit |
| >10% | Skin fold remains tented, sunken eyeballs, dry mucous membranes | Maintenance requirement 50ml/kg + 100-120ml deficit |
| >12% | Like 10-12%, but life-threatening, circulatory collapse | Maintenance requirement 50ml/kg + 120-150ml deficit |





Nutrition and Care for Kidney Diseases
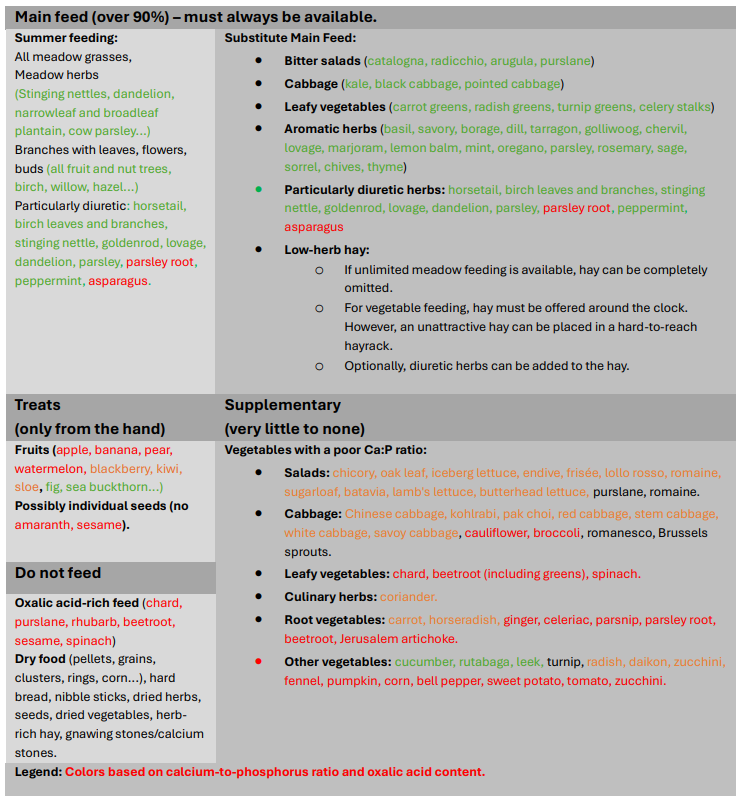
Pure fresh feeding
In cases of kidney insufficiency, it is especially important that rabbits consume a lot of water during treatment and for years afterward, as it flushes the organs and helps expel calcium, preventing its deposition and easing the burden on the kidneys. Therefore, rabbits should be provided with fresh, varied, and mostly leafy foods ad libitum (in unlimited amounts, available at all times), as these provide the most water.
Rabbits affected by such conditions or prone to them should be fed a varied fresh diet (preferably with meadow herbs in summer, and leafy vegetables, herbs, and minimal fruit in winter). Hay should be offered additionally, but ideally, enough fresh food should be provided so that they hardly need to eat hay. Avoid using hay that is too herb-rich. Dry herbs should not be offered. Seeds, grains, hard bread, chewing sticks, snacks/treats, and dry food put strain on the kidneys and should never be given.
Increasing Water Intake and Drinking
It is also important to offer water at all times in a clean bowl (it has been proven that less water is consumed from nipple drinkers).
To increase water intake, diluted carrot juice, vegetable juice, or pure fruit juice (not nectar) can be offered, diluted with water. Pure herbal tea (if it is liked) is also useful. A medicinal kidney and bladder tea, such as HEUMANN Bladder and Kidney Tea SOLUBITRAT®, is a good option. These drinks should always be available in addition to water and not as a replacement.
Diuretic Herbs
Supporting the treatment with diuretic herbs is beneficial, such as nettles (let them wilt for about 1 hour to prevent them from stinging), birch leaves and bark, horsetail, asparagus (if they eat it), true goldenrod or giant goldenrod, dandelion, parsley root, and lovage.
Correcting Vitamin D Deficiency
For indoor rabbits, ensure that they receive adequate vitamin D. Most rabbits in indoor housing or dark enclosures suffer from a significant deficiency. Window glass blocks UV-B rays, which are necessary for rabbits to produce vitamin D in their bodies. Use fortified food or, even better, a UVB lamp, or provide your rabbits with access to direct sunlight for longer periods each day without glass in between (open windows, balcony access, outdoor enclosures…). In cases of kidney insufficiency, vitamin D can be very poorly synthesized, making this aspect even more crucial.
Feeding Low Calcium?
Please do not make the mistake of feeding a low-calcium diet. Unfortunately, this is still recommended in many places, but it is harmful to the rabbit’s health and does more harm than good (this is not to say that you should offer them excessive amounts of calcium-rich foods). Rabbits have a high calcium requirement for their continuously growing teeth, and deficiencies can lead to dental issues and other health problems. However, excess calcium is also not advisable! Dry foods should be avoided as they lead to a high calcium concentration (such as dry food, dry herbs…). Instead of extremely herb-rich or leaf-rich hay, offer less popular hay without additives. It is very important to pay attention to the calcium-phosphorus ratio.
Calcium-Phosphorus Ratio:
Ensure a balanced calcium-phosphorus ratio of 1.5-2:1 (Ca: P) in your rabbit’s diet or feed them exclusively with meadow plants (available at all times, day and night) or other green forage, without adding other foods. Make sure that the ratio is balanced in the overall diet, not just in individual components. You need to be especially careful with the calcium-phosphorus ratio if you supplement the rabbit’s diet with hay rather than feeding them solely green food, as this reduces their water intake. Also, if urinary tract issues arise, even with a purely meadow-based diet (such as a strong predisposition to grit and stones), you should be cautious.
If the phosphorus content in the diet is too high, the body compensates by breaking down calcium from bones and teeth. If the phosphorus content is too low, calcium will not be adequately integrated into the bones and teeth. If the calcium content of the food is too high, stones and grit can form. However, reducing calcium in the diet is absolutely not recommended, even though it is commonly suggested. A calcium-reduced diet leads to calcium deficiency, which can also cause kidney stones and bladder grit, along with weak bones and thin or brittle teeth.
No Excess Protein, But Not Protein-Deficient
Protein consists of amino acids, which must be consumed in amounts that meet the rabbit’s nutritional needs. Foods with good amino acid profiles are recommended, and it is advisable to consult with a nutritionist. Excess protein is harmful to the kidneys and should be checked via blood tests.
Feed Low Phosphorus
Phosphorus also stresses the kidneys. Phosphorus-rich foods overly burden the kidneys and can shorten the lifespan. Foods high in phosphorus include seeds, grains, and even certain types of cabbage, so these should make up no more than a quarter of the diet.
Case Report: Acute Renal Failure in Henri
Henri was severely dehydrated, weighing 1.46 kg (instead of 1.8 kg). Diagnosis was confirmed through a blood test during an emergency veterinary visit. He received two days of inpatient care, including infusions, kidney ultrasounds (to rule out structural damage), and repeated blood tests. After 14 days, a follow-up check showed improvement, and Henri was healthy again.
Today, 8 months later, Henri weighs 1.9 kg and is doing well.
„The emergency vet wanted to euthanize him, but I took him home overnight and the next day, I brought him to a rabbit specialist, which saved his life.“


Sources include:
Binder, N. (2011): Referenzbereiche für Urinparameter bei Kaninchen und Meerschweinchen. lmu München
Ewringmann, A. (2016): Leitsymptome beim Kaninchen: Diagnostischer Leitfaden und Therapie. Georg Thieme Verlag
Glöckner, B. (2015): Nierenerkrankungen beim Kaninchen–Ursachen und Therapiemöglichkeiten. kleintier konkret, 18(S 02), 3-10
Hein, J. (2015): Urinuntersuchung beim Kleinsäuger–so einfach und doch so aussagekräftig. kleintier konkret, 18(S 01), 30-35.
Lazarz, B., & Rother, N. (2017): Nephrotomie beim Kaninchen–Ein Fallbericht. kleintier konkret, 20(S 01), 13-17.
Madel, A. (2016). Untersuchungen zur Azotämie bei Heimtierkaninchen, Freie Universität Berlin
Meredith, A., & Lord, B. (2014). BSAVA manual of rabbit medicine. British Small Animal Veterinary Association
Praag, van E. (2017): Nephrolithen und Urolithen (Nieren- Blasen- und Harnröhrenstein bei Kaninchen). [http://www.medirabbit.com/GE/Urogenital/Stones/Urolithias_ge.htm, 13.09.2017]
Varga, M. (2014): Textbook of Rabbit Medicine. Second Edition
Wolf, P., Cappai, M. G., & Kamphues, J. (2020): Water consumption in small mammals (dwarf rabbits, Guinea pigs and chinchillas): New data about possible influencing factors. Research in veterinary science, 133, 146-149.




















