Contents
- Encephalitozoonosis Cuniculi(E. cuniculi, Encephalitozoonosis, Encephalitozoon cuniculi, EC)
- What is E. cuniculi?
- How Many Rabbits Carry the Pathogen?
- Triggers
- Transmission Pathways
- Is E. cuniculi Contagious to Other Rabbits?
- A New Rabbit is Joining?
- Can Rabbit Owners Get Infected by Their Rabbits?
- Symptoms: How to Recognize E. Cuniculi?
- Head Tilt
- Paralysis Symptoms
- Seizures & Cramps with Disorientation
- Eye Diseases (Uveitis, Cataracts, Glaucoma), Eye Tremors, Delayed Pupil Reflex
- Nystagmus (Eye Movements):
- (Unilateral) „Facial Paralysis“ and Raised Mouth Corner
- Head Tilting and Raising the Head
- Coordination and Posture Disorders (Ataxia)
- Scanning (Compulsive Head Movement in Resting Position)
- Incontinence
- Kidney Insufficiency and Organ Damage (e.g., Increased Thirst, Dull Coat, Lethargy, Loss of Appetite)
- Chronically Weakened Immune System: Susceptibility to Other Diseases, Persistent Illnesses, the Animal Does Not Recover
- Diagnosis of E. Cuniculi Infection
- Distinguishing Between E. Cuniculi and Ear Infections in Rabbits: Symptoms, Diagnosis, and Treatment
- Treatment
- Treatment of Head Tilt, Balance Disorders, Seizures & Paralysis
- Treatment of Other Symptoms
- How long should I fight and when should I let go?
- Proper Care
- Experience Report: Partner Rabbit with E. Cuniculi Rabbits
- Hand-feeding and food intake
- Prevention
- Disinfection
- Case Reports
Encephalitozoonosis Cuniculi
(E. cuniculi, Encephalitozoonosis, Encephalitozoon cuniculi, EC)
Since the disease is sometimes associated with a tilted head, it is also symptomatically referred to as Head Tilt Disease, Star-Gazer Disease, Moon-Gazer Syndrome, or simply as „head tilt“ or torticollis.

What is E. cuniculi?
The complicated name “E. cuniculi” refers to a pathogen that frequently causes disease in rabbits. Typical symptoms primarily affect well-perfused organs, particularly:
- The central nervous system (e.g., head tilt, paralysis, rolling, circling, uncontrolled eye movements, incontinence).
- The eyes (e.g., cataracts, uveitis, glaucoma).
- The kidneys, and in some cases:
The heart, digestive organs, lungs, and liver.
E. cuniculi can lead to a variety of serious health issues in rabbits, often requiring prompt veterinary attention.
How Many Rabbits Carry the Pathogen?
Approximately 18-40% of healthy pet rabbits in Germany carry the E. cuniculi pathogen. These animals are latently infected, meaning the pathogen or antibodies against it can be detected, but the rabbits themselves show no visible symptoms.
Among entirely healthy rabbits, the prevalence rate is lower. A study from Bavaria found that 18% of rabbits were infected. In studies including both sick and healthy rabbits, the prevalence rate was slightly higher, around 35-40% among all animals, compared to 48-56% among only sick rabbits.
In many breeding operations, targeted selection efforts have reduced the prevalence rate to below 10%. Since E. cuniculi can be transmitted in utero, testing parent animals is essential. Similar strategies have also brought the prevalence rate in laboratory rabbit breeding to below 10%.
Interestingly, a study by Meyer-Breckwoldt (1996) indicated that wild rabbits in Germany are not affected by E. cuniculi. However, other research has documented E. cuniculi infections in wild rabbits, suggesting that the presence of the pathogen in wild populations may vary depending on the study and location.
Triggers
Rabbits with a normal immune system typically keep the E. cuniculi pathogen under control, preventing it from causing clinical symptoms. However, if the immune system becomes compromised, the pathogen can multiply rapidly, leading to signs of disease.
Rabbits are particularly at risk in stressful situations, such as:
- Bonding with new companions.
- Loss of a bonded partner.
- Exposure to severe weather (e.g., storms, thunderstorms).
- New Year’s Eve fireworks.
- Being kept in isolation or poor living conditions.
Other risk factors include:
- Existing illnesses.
- Administration of corticosteroids, which can weaken the immune response.
- Advanced age, as older rabbits are statistically more vulnerable than younger ones.
In such cases, the pathogen may proliferate shortly after the triggering event or even days later, causing damage to the central nervous system or organs, resulting in symptoms.
It is important to note, however, that not all rabbits exposed to these situations experience an outbreak. Many rabbits endure similar stressors without developing acute symptoms, suggesting that individual factors, including overall health and genetics, play a role in susceptibility.
Transmission Pathways
E. cuniculi is primarily transmitted through urine. Infected rabbits periodically shed spores in their urine, even if they appear clinically healthy. Other animals, such as guinea pigs, are also potential carriers of the pathogen.
Rabbits ingest the spores through grooming or by consuming food contaminated with urine. Once ingested, the spores infect the rabbit via the digestive tract. This can lead to reinfection, further intensifying the burden of the pathogen.
Other transmission pathways include:
- In utero transmission via the placenta.
- Inhalation of infected droplets or dust particles.
- Transmission via feces is debated among experts.
Once a rabbit is infected, it carries the pathogen for life, as the infection is typically chronic and cannot be completely eliminated.
Is E. cuniculi Contagious to Other Rabbits?
The majority of rabbits that come into contact with an infected rabbit already carry the E. cuniculi pathogen, as they were likely exposed at some point. For this reason, untested companions are generally assumed to be carriers. The risk of transmission in such cases is not higher than it has been in the past.
Separation of rabbits is not recommended, as the sick rabbit relies on the presence of its social partner(s) to recover. Social isolation can cause additional stress, which may hinder recovery.
The only exception is if the sick rabbit is being severely bullied or injured by its companions. In such cases, a careful assessment is necessary to determine whether the stress of losing its partner is less harmful than the stress caused by conflicts.

Important!
Unfortunately, far too many sick rabbits are still being separated from their companions. Always ensure that at least one companion stays with the sick rabbit.Rabbits are highly social animals, and the presence of a partner is crucial for their mental well-being and recovery. Separation can cause significant stress, which may worsen the rabbit’s condition.
A New Rabbit is Joining?
If you have a rabbit infected with E. cuniculi, it is recommended to only introduce other infected rabbits to avoid transmitting the pathogen to new, uninfected rabbits.
A blood test (IgG titer) can help determine which rabbits are E. cuniculi carriers and which are not. This ensures that you can make informed decisions about introducing new companions while minimizing the risk of spreading the infection.

Can Rabbit Owners Get Infected by Their Rabbits?
E. cuniculi is a zoonotic pathogen, meaning transmission to humans is theoretically possible. However, documented cases of human infection have only occurred in individuals with weakened immune systems, such as those with:
- HIV/AIDS
- Undergoing chemotherapy
- After organ transplantation
Precautions for At-Risk Groups:
People in these high-risk groups should avoid contact with rabbits unless infection in the rabbit has been ruled out through a blood test.
Facilities such as nursing homes, kindergartens, and similar institutions should only keep rabbits that have been proven E. cuniculi-free.
Testing for Humans:
A human infection can be tested through stool samples, which can be analyzed by tropical medicine institutions.
For Healthy Individuals:
For healthy people, the risk of infection is extremely low with proper hygiene practices. Even clinically healthy rabbits can be carriers of E. cuniculi, meaning they can spread the pathogen regardless of visible symptoms.
Importantly, a rabbit currently showing symptoms is no more contagious than it was in the past, before the disease became evident. Thus, there is no heightened risk from a sick rabbit compared to when it was asymptomatic.
Symptoms: How to Recognize E. Cuniculi?
E. cuniculi is a complex disease that can manifest in a variety of ways. The most common symptoms affect the central nervous system, eyes, and kidneys. Typically, only one or a few symptoms are present at a time.
In a study conducted by the Veterinary University of Vienna, involving 144 rabbits with clinical signs of E. cuniculi, the following symptoms were observed:
- 75% showed neurological symptoms (e.g., head tilt, paralysis, uncoordinated movements, or seizures).
- 14.6% had uveitis (inflammation of the eye).
- 3.5% showed signs of kidney failure.
Only 6.9% of the rabbits exhibited a combination of multiple symptoms.
Important!
Rabbits affected by E. cuniculi typically show only one of the possible symptoms at a time. For example, they may simply have urinary incontinence (being unclean) or experience paralysis in the hind legs.This means that the disease can present in a subtle or isolated way, and not all rabbits will show multiple symptoms at once. It’s essential to look out for any signs of abnormal behavior or physical changes, and seek veterinary care if any concerning symptoms appear.
Head Tilt
Head tilt is one of the most commonly recognized symptoms of E. cuniculi, but it does not affect all rabbits with the disease. In affected rabbits, the head is tilted to one side, and the degree of the tilt can vary significantly from hour to hour or day to day. Some rabbits may show a head tilt only occasionally, while others may maintain a persistent tilt.
While head tilt is often associated with E. cuniculi, it is more commonly caused by ear infections, particularly otitis (inflammation of the ear). Only a smaller percentage of head tilt cases are directly caused by E. cuniculi.
Other Possible Causes of Head Tilt:
- Middle or inner ear infections (otitis media or interna).
- Meningitis (inflammation of the brain lining).
- Toxins or poisoning.
- Injuries (e.g., from accidents).
- Abscesses (e.g., dental abscesses or in the neck or head).
- Stroke, brain tumors, or larva migrans (parasitic infection).
- Listeriosis, toxoplasmosis, or herpes (rare but can lead to head tilt, especially in acute, often fatal cases).

Diagnostic Approach:
To diagnose the cause of head tilt, a veterinarian will typically start by performing:
- Blood tests to detect E. cuniculi (IgG titer).
- Neurological examination to assess the nervous system.
It’s essential to exclude ear infections, as they are more common than E. cuniculi in causing head tilt. Advanced imaging techniques like MRI (Magnetic Resonance Imaging) or CT scans (Computed Tomography) are preferred over X-rays, as they provide more detailed information and are better at detecting issues in the ear and brain.
Paralysis Symptoms
One of the most common signs of E. cuniculi is paralysis of the hind legs, which may result in the legs being dragged behind the rabbit. However, unlike a true paralysis, the reflexes in the foot are still present. Other forms of paralysis or weakness can also occur.

In addition to E. cuniculi, many other conditions can cause paralysis symptoms in rabbits, including:
- Arthritis (Arthrose), spondylosis, or hip dysplasia (HD).
- Toxoplasmosis.
- Bone fractures or spinal injuries.
- Meningitis (inflammation of the brain lining).
- Brain damage.
- Central nervous system diseases.
- Hypokalemia or hyperkalemia (low or high potassium levels).
- Hypermagnesemia (elevated magnesium levels).
- Vitamin E deficiency.
- Abscesses or tumors pressing on nerves.
- Hyperthyroidism (overactive thyroid).
- Vertebral inflammation.
- Heart diseases.
- Coccidiosis (intestinal parasitic infection).
- Pneumonia.
- Listeriosis (bacterial infection).
- Larva migrans (parasitic infection).
- Severe bladder grit or kidney stones.
- Diseases causing pain in the spine or legs (e.g., pododermatitis, abscesses).
- Floppy Rabbit Syndrome (neurological disorder).
- Infectious bone or joint diseases.
Diagnostic Approach:
To diagnose the underlying cause of paralysis, the following steps are essential:
- X-rays taken from two different angles to assess bone and joint health, and to rule out fractures or vertebral issues.
- A complete blood count (CBC), along with titer testing (IgG) to check for E. cuniculi infection.
Additional tests or imaging (such as an MRI or CT scan) may be needed depending on the suspected condition.
A thorough diagnostic approach is crucial to accurately identify the cause and determine the most appropriate treatment for the affected rabbit.

Seizures & Cramps with Disorientation
Rabbits affected by E. cuniculi may experience seizures, muscle cramps, and episodes of disorientation. During these episodes, they may lose their sense of direction, fail to respond to external stimuli, or react with delayed responses. They may twist their bodies, causing them to roll uncontrollably, and display nervous and uncontrolled eye movements, staring blankly or convulsing.
Other Possible Causes of Seizures and Cramps:
In addition to E. cuniculi, many other conditions can cause similar symptoms:
- Coccidiosis (especially in young rabbits).
- Breed-specific scanning behavior in certain white rabbit breeds.
- Herpesvirus infections.
- Toxoplasmosis.
- Epilepsy.
- Meningitis (inflammation of the brain lining).
- Injuries (e.g., accidents).
- Ear infections.
- Heart diseases.
- Poisoning (from toxins).
- Kidney diseases.
- Brain tumors or abscesses.
- Death convulsions in the final stages of severe illness.
Diagnostic Approach:
Seizures and muscle cramps require careful diagnostic evaluation, as there are many potential causes. Diagnosis depends on the specific symptoms observed, and a rabbit-experienced veterinarian should be consulted. Further tests such as bloodwork, imaging (e.g., X-rays, MRI), and other relevant examinations may be necessary to determine the cause.
If your rabbit is experiencing seizures or disorientation, it is important to act quickly and seek professional care to identify and address the underlying issue.

Eye Diseases (Uveitis, Cataracts, Glaucoma), Eye Tremors, Delayed Pupil Reflex
E. cuniculi can affect the eyes in several ways, leading to various eye diseases. If a rabbit is infected in utero (while still in the womb), the pathogen can settle in the lens capsule, which is still underdeveloped at this stage. This can later result in uveitis (inflammation of the eye), which typically presents as a white film or cloudiness over the eye, sometimes even covering the pupil. Additionally, reddish-white spots may be visible on the eye.
If left untreated, or if treatment is ineffective, further complications can arise, including:
- Cataracts (clouding of the lens, leading to impaired vision).
- Glaucoma (increased pressure in the eye, which can lead to blindness if untreated).

Nystagmus (Eye Movements):
During acute outbreaks, rabbits often experience uncontrolled eye twitches or movements (nystagmus) and a delayed pupil reflex (where the pupil reacts slowly to movements in front of the eye). In E. cuniculi (EC), the nystagmus is typically vertical (up and down), whereas in an ear infection (otitis), it is horizontal (side to side). However, many rabbits with otitis also experience an E. cuniculi outbreak due to immune weakness. Therefore, a vertical eye movement does not rule out the possibility of otitis!
In rabbits affected by E. cuniculi, it is common for them to sustain injuries to their eyelids, cornea, and conjunctiva. This often occurs because the rabbit may roll uncontrollably due to neurological issues, causing them to injure their eyes against the ground or other surfaces during these episodes of „culling“ (rolling).
(Unilateral) „Facial Paralysis“ and Raised Mouth Corner
A raised corner of the mouth (ipsilateral hemifascicular spasm, often mistakenly called facial paralysis) is not typically a symptom of E. cuniculi, but rather a sign of an ear infection (otitis). The opposite corner of the mouth may appear „droopy“ or lower than usual. This can be misunderstood as a facial paralysis, but it is actually associated with issues in the ear, such as inflammation or infection, which affect the facial nerve.

Spasm of the facial nerve leads to an elevated corner of the mouth on the affected side.
Head Tilting and Raising the Head
In most cases, when rabbits tilt their heads back or raise their heads, it is a sign of difficulty breathing caused by a heart or lung condition (such as fluid in the lungs). This situation is considered an emergency, and it is crucial to seek immediate veterinary care, where X-rays from two different positions should be taken to rule out fluid in the lungs.
If no fluid is found in the lungs, a heart ultrasound should be performed to check for heart issues.
It is only in very rare cases that rabbits with E. cuniculi will occasionally tilt their heads back, typically in stressful situations. This behavior would be sporadic (happening occasionally) rather than continuous.
Coordination and Posture Disorders (Ataxia)
Many rabbits with E. cuniculi (ECl) exhibit lack of coordination or appear clumsy, often injuring themselves or moving in a strange or unusual manner compared to their healthy counterparts. They may adopt odd body postures or show signs of increased muscle tension, such as spreading their legs when lifted. These can be clear indications of ataxia (a loss of coordination) caused by neurological impairment due to the infection.
Scanning (Compulsive Head Movement in Resting Position)
Scanning refers to the behavior where a rabbit moves its head back and forth compulsively while at rest. This can sometimes be observed in rabbits infected with E. cuniculi, but it is also a breed-specific trait. It is particularly common in white rabbits, Siamese, Russian rabbits, and their mixes, where this behavior occurs naturally and is not necessarily linked to an underlying health issue.
In the case of E. cuniculi infection, scanning could be a sign of neurological involvement, but when it occurs in specific breeds, it may simply be part of the breed’s typical behavior.
Incontinence
During acute outbreaks of E. cuniculi, affected rabbits may experience incontinence, meaning that previously litter-trained rabbits suddenly become unclean. It is also common for there to be a significant increase in urine volume, or the rabbit may drink much more water than usual. However, with successful treatment, this incontinence typically resolves.
Other possible causes of incontinence in rabbits include:
- Urinary tract diseases (such as urinary or bladder infections, urinary stones, kidney stones, kidney gravel, kidney insufficiency)
- Spinal disorders (including spondylosis, arthritis, vertebral fractures, dislocation of the spine)
- Nerve damage
- Pregnancy
- Obesity
- Pain
- Post-castration effects
- Increased urine volume (due to conditions like diabetes or kidney insufficiency)
- Toxoplasmosis
- Lungworms
Kidney Insufficiency and Organ Damage (e.g., Increased Thirst, Dull Coat, Lethargy, Loss of Appetite)
E. cuniculi can affect the entire body and often leads to kidney insufficiency, as well as damage to the heart muscle and liver. The strain on the kidneys is often noticeable during acute outbreaks, as there is increased water intake, leading to more urine output. A healthy rabbit with a diet of fresh greens generally drinks very little. So, if your rabbit is drinking more, kidney insufficiency is likely.
Chronic kidney dysfunction can cause deposits in the urinary tract, as the kidneys are not being flushed effectively. In E. cuniculi-positive rabbits, it is important to regularly check kidney function, as early treatment can save lives. Rabbits do not die directly from E. cuniculi, but often from undiagnosed or late-diagnosed kidney insufficiency.

Diagnosis:
- A complete blood test is necessary to assess kidney function, with creatinine and urea being key indicators of kidney insufficiency.
- Ultrasound can show the extent of kidney damage.
Early detection and treatment of kidney insufficiency can significantly improve your rabbit’s prognosis.
Chronically Weakened Immune System: Susceptibility to Other Diseases, Persistent Illnesses, the Animal Does Not Recover
A chronically weakened immune system makes the rabbit more vulnerable to other illnesses, leading to ongoing health problems. The animal may struggle to recover and remain in a state of persistent illness.
Diagnosis of E. Cuniculi Infection
Important! Please make sure to visit only veterinarians who are knowledgeable about rabbits! In veterinary studies, rabbits are only a peripheral topic, which is why only veterinarians who specialize in this species are suitable!
For a rabbit-experienced veterinarian, blood tests and X-rays are standard procedures. Even if the symptoms „look exactly like E. Cuniculi,“ a recent study shows that around 70% of these animals actually had another disease or a completely different condition as the cause. Many of these diseases are very painful or fatal, causing the animals to suffer unnecessarily for months or years, or they may die. Only with the correct diagnostics can the rabbit be protected from suffering or death.
The following examinations are important:
- A blood check should generally be performed at an external laboratory (IgG titer, kidney values, CK (trauma), differential blood count (inflammation), liver values) to rule out differential diagnoses and check liver and kidney function. A positive IgG titer indicates that the rabbit carries the pathogen, but the disease may still be caused by something else. The level of the IgG titer does not indicate whether the animal is acutely affected by E. Cuniculi; it only shows whether the rabbit carries the pathogen and should be tested once in its lifetime if it is positive. Most rabbits have a high titer for life, which is necessary to protect the animal. Therefore, all possible diagnoses must be ruled out! For a long time, it was believed that the IgM titer indicates an acute disease, but recent studies show that this is not the case. If a rabbit is EC-positive (IgG titer), it does not mean that the symptoms are caused by EC, as the rabbit could also have two diseases at once. Since about 40% of rabbits are EC-positive and these rabbits can also have ear infections, all other possible causes must always be ruled out before a diagnosis is made. E. Cuniculi itself does not lead to any changes in the blood count, nor does it cause an inflammatory reaction (pseudoleukocytosis…). Only when the kidneys are severely damaged can mild anemia or elevated creatinine and urea levels occur. The CK value may be elevated in extreme cases due to running and rolling, otherwise, it is more likely to indicate a differential diagnosis (trauma). All other blood count changes usually occur when another disease has caused the symptoms or when secondary infections arise.
- X-rays are often necessary, especially in cases of paralysis and head tilting (ear infections, skull trauma). A CT scan is superior to X-rays.
- A thorough general examination should be standard practice: Head tilt – check the ears, teeth, mouth, and head; is there a fever? Eye injuries from rolling?
- Paralysis: Check the soles of the feet, spine, heart, and look for signs of fever.
- Additional investigations may be important, depending on the direction of the suspicion and the symptoms presented. Please refer to the guidelines for each specific symptom!

Distinguishing Between E. Cuniculi and Ear Infections in Rabbits: Symptoms, Diagnosis, and Treatment
E. cuniculi and ear infections share similar symptoms but require different treatments. Both conditions can cause head tilt, rolling, seizures, and eye movements. In rabbits that test positive for EC, ear infections often develop as a secondary issue, as the E. cuniculi parasite takes advantage of the weakened immune system.
At the veterinarian: The middle and inner ear are located behind the eardrum, which means inflammation cannot be seen simply by looking into the ear. In addition to the EC titers in the blood and a neurological examination, an ear infection should always be ruled out through imaging techniques, with a CT scan being superior to X-rays.
Treatment
In the case of an acute outbreak of E. Cuniculi, every minute counts. The earlier the correct treatment is started, the higher the chances of success.
The pathogen cannot be completely eradicated through treatment, but the symptoms can be improved or cured, and the pathogen can be suppressed.
There is ongoing debate about whether partner rabbits need to be treated as well.
Depending on the symptoms, different treatments are required

Treatment of Head Tilt, Balance Disorders, Seizures & Paralysis
Medication Recommendations:
- Panacur (administered daily and consistently for 14-28 days, or longer if the rabbit is still in the acute phase at that time) has been proven effective in multiple studies. It kills spores in the intestines, thus relieving the immune system. Oxfendazole and Albendazole are also effective but are less well tolerated than Fenbendazole. For gentle, stress-free administration, refer to specific guidelines.
- Antibiotics to Combat Secondary Infections (Oxytetracycline, Chloramphenicol, Gyrase inhibitors like Baytril):
Oxytetracycline and Chloramphenicol should only be used if kidney and liver function are proven to be intact. Generally, Baytril is sufficient as a well-tolerated antibiotic. The antibiotic is given to prevent secondary infections (e.g., kidney infections, which are common with E. Cuniculi), which are conditions that arise as a consequence of the infection. Normally, it is administered for at least 10 days, but it may be extended if well tolerated, or shortened if poorly tolerated. Depending on the severity of the disease, the antibiotic may sometimes be omitted. To reduce stress and keep digestion stable, it may be helpful to learn how to administer the antibiotic via injection into the skin.
- Corticosteroids are not necessary and can be harmful if E. Cuniculi is the actual cause. Studies show that corticosteroids have no effect on the disease and do not work against it. Although there is often an initial improvement when corticosteroids are used, rabbits treated with them do not recover faster nor have a higher survival rate. Research has shown that rabbits receiving corticosteroids showed no advantages compared to those who did not. Furthermore, corticosteroids put significant strain on the liver (which is often already severely affected by E. Cuniculi), cause a significant increase in the E. Cuniculi pathogen, and make the rabbits more susceptible to other infections. Corticosteroids can increase the overall mortality rate after the disease. Some veterinarians may use corticosteroids as a last resort before euthanasia, after all differential diagnoses have been carefully excluded and no success has been achieved with standard treatments over several weeks. In such cases, additional support with Zylexis, milk thistle seeds or extracts, and Hepar comp. should be administered.
- High-dose Vitamin B12 or Vitamin B complex (available at pharmacies or specially for rabbits online) can help regenerate the nerves. This should be given until the seizures, head tilt, or paralysis completely resolve, and symptoms often continue to improve over weeks. Initially, it is best to administer it as an injection at a high dose, and later, it can also be given as drops, for example, mixed with the Panacur paste. If infusions are administered, the Vitamin B can be added to the infusion, so only one injection site is needed, preventing any discomfort from multiple injections.
- Try to find fresh cow parsnip (Heracleum sphondylium) in the meadow and offer it to the rabbits.
- Additionally, the immune system should be supported, as it is crucial for containing the pathogen. There are many options for this. Zylexis, in particular, can be administered by the veterinarian.
- Homeopathically, Cerebrum comp. can be used for nerve system regeneration (if these symptoms are present), Vertigoheel for dizziness, and Engystol for the immune system. These can also be added to the infusion.
- Physiotherapy, including gentle movements of the paralyzed limbs, is essential to prevent stiffness and muscle atrophy, as without it, the rabbits have no chance of recovery. In cases of paralysis, the legs must be moved several times a day, either through physiotherapy or, ideally, through the rabbit’s own movements on a firm surface with enough space. Exercises:
Even with head tilt, massages and physiotherapy are beneficial to keep the neck flexible.
- Infusions (e.g., can be ordered online) are important, as the pathogen tends to accumulate in the kidney tissue. Infusions help prevent kidney failure or damage, as well as the later development of kidney disease as a consequence. Unrecognized kidney insufficiency is the leading cause of death in E. Cuniculi cases. If the rabbit refuses food, infusions should be given twice daily. However, it is essential to weigh whether the stress of daily vet visits is more harmful than the benefit of the infusions. If possible, infusions can be administered at home, provided the veterinarian demonstrates how to do so (see video).

- A remedy for nausea and dizziness, especially if the rabbit is flipping over or has uncontrolled eye movements, includes medications like Vomex A (Dimenhydrinate), or depending on the case, Cerenia (Maropitant) or Emeprid (Metoclopramide).
- Offering or administering diluted vegetable and fruit juices (pure juice made from 100% fruit/vegetable, not nectar) can also help increase fluid intake. For example, a bowl of carrot juice.
- The flushing out of the pathogens can be supported by a diet rich in fresh foods. During the summer months, affected rabbits should be fed exclusively with fresh wild herbs, tree leaves, and grasses. Especially valuable are diuretic herbs such as dandelion, lovage, birch, parsley, dill, sorrel, nettle, ground elder, and others.

Treatment of Other Symptoms
The administration of Panacur is also very important for other symptoms.
For epileptic seizures and cramps, in addition to Panacur, Vitamin B complex should definitely be injected. Benzodiazepines (e.g., Diazepam, Midazolam) are often used as well.
Eye diseases, such as uveitis, are usually treated symptomatically with tetracycline-based eye drops or ointments, as well as corticosteroid-containing eye drops and ointments, in addition to Panacur. Unfortunately, Panacur does not work in the eye, but it should still be administered to reduce the pathogen load.
For kidney insufficiency, the treatment is described here.
Important: It is completely normal for the symptoms to continue worsening after the treatment begins. Stabilization typically occurs much later

How long should I fight and when should I let go?
As long as the rabbit is fighting the illness on its own, meaning it is still eating when offered food or syringe feeding, please continue to fight alongside your rabbit and support it! E. Cuniculi is difficult to witness and endure, and the thoughts of „euthanasia“ often arise. However, with proper medication, the right care, and minimal stress (which is very important for E. Cuniculi!), most rabbits make it through. Moreover, they experience no pain, provided the condition is truly caused by E. Cuniculi.
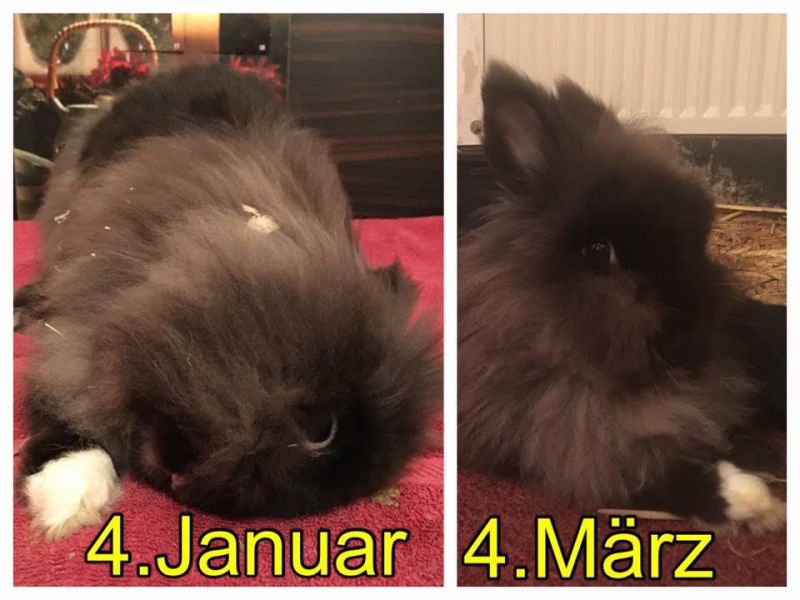
Most rabbits with E. Cuniculi are euthanized, even though they are still fighting. The first two photo examples below should have been euthanized according to the veterinarians’ opinion, but against their advice, they were successfully treated. Some rabbits retain a slight head tilt, but can straighten their head when needed (e.g., to eat) and are able to do everything that rabbits enjoy doing (e.g., running, digging, jumping), or are only mildly restricted. Normally, the condition of sick rabbits worsens during the first few days or even weeks, despite treatment. Eventually, a plateau is reached, and later on, very slow progress can be seen. The rabbits no longer have balance problems but may only have residual effects from the illness (e.g., a tilted head). Over time, these symptoms will decrease and eventually disappear entirely. If after about three months no improvement is seen, medication can be changed.
Important: Unfortunately, there are still people who want to save costs and avoid diagnostics. Diagnostics save lives! There are many rabbits that are treated for E. Cuniculi for months, but actually have something entirely different (e.g., apparent paralysis due to a spinal fracture, head tilt caused by ear infections, etc.). Even if the treatment seems to improve the condition initially, always have a blood test with a titer measurement (IgG) done. Rabbits with movement disorders, head tilt, or paralysis should be X-rayed, etc. These animals suffer from pain, and due to the prolonged misdiagnosis, they often must be euthanized. This is not acceptable!
Rabbits with E. Cuniculi have good chances of recovery. In some cases, however, euthanasia may be the right decision. We frequently take in rabbits for care until they are healthy and thus constantly deal with E. Cuniculi cases. In addition to proper diagnostics, correct treatment, absolute stress-free care, and an optimal environment, patience is required. This experience has also removed the fear of the disease and motivated us to create this extensive website with tips. Our own group of nine rabbits is led by one who had a severe E. Cuniculi outbreak years ago, resulting in complete paralysis of her hind legs. She is now completely healthy, an expert escape artist, and has no limitations. The veterinarian wanted to euthanize her and gave us no hope, but we pursued the proper treatment against the vet’s advice.
However, if you are not capable of or unwilling to provide intensive care and the proper diagnostics, euthanasia is often the kindest option, as anything else would be animal cruelty. Only through intensive care will the rabbits recover.
Proper Care
Important! Proper care is crucial for the recovery of rabbits with E. Cuniculi.
- No stress, as it can significantly affect E. Cuniculi and rapidly worsen the condition. Medications should be administered at home, as frequent vet visits often lead to deterioration. A thorough diagnosis should be done initially, and only if the condition worsens or new symptoms arise (e.g., changes in the eyes) should a follow-up visit be necessary. After cleaning, everything should be returned to its original place. The substrate or bedding should not be drastically changed, and cleaning should only be done when necessary (remove leftover food and major waste daily, and ideally clean only one part of the area at a time rather than doing everything at once).

- When choosing bedding, be sure to consider the risk of eye injury during „binkying“ (jumping). Use towels, VetBeds, or other soft fabrics, and regularly check the eyes for any signs of injury.
- The medications must be administered consistently.
- The rabbit must be cared for to prevent other illnesses from developing (e.g., clean its bottom with baby wipes if it becomes soiled). Since incontinence is often present, it’s crucial to ensure that the rabbit always has a dry surface, as otherwise, it can quickly develop urinary tract infections.
- Handling rabbits with E. Cuniculi is not easy, as they can quickly lose their sense of orientation and should not be lifted, moved, or carried. Therefore, it’s helpful to provide a transport box or crate in the enclosure. If the rabbit needs to be taken to the vet, it can be lifted using this box. A cloth over the box can have a calming effect, as it provides a sense of security from the familiar environment. Medications should be administered without lifting the rabbit. If lifting is unavoidable (e.g., to clean the bottom from feces and urine), lift the rabbit gently but firmly, and always cover its eyes with a hand or cloth to calm it. When setting it down, stay close and offer support with your hands until the rabbit regains its balance and orientation.
- Keep the partner rabbit with the sick rabbit! Do not separate them unless the partner is aggressive towards the sick rabbit (e.g., biting). The presence of the partner rabbit is crucial for stabilization and healing, as it helps reduce stress (which is often underestimated). In groups, either separate the affected rabbit with the one it gets along with best or keep it within the group (if the group is harmonious).
- Ideally, the rabbit should stay in its familiar environment. Potential hazards, such as sharp objects and other dangers, should be padded or removed. Often, it is sufficient to adjust part of the enclosure and create a small barrier to separate the sick rabbit from the rest of the enclosure (e.g., using a rolled-up blanket or low boundaries). The sick rabbit won’t be able to overcome it, but the healthy ones can. A large cage tray works well for this purpose.
Experience Report: Partner Rabbit with E. Cuniculi Rabbits
Two years ago, Leo developed a head tilt. Naturally, Leo would fall over, roll, and was really confused and withdrawn. At first, Lisa somehow thought it was a sign of aggression, so she would run over to him, growl, and bite him – which was, of course, really upsetting for both me and Leo. But I guess she was just confused about what was going on. It didn’t take long for her to realize that Leo was actually sick. Soon after, every time Leo rolled, she would run over and sit on the side he was rolling towards to stabilize him. Even when they were just sitting together, she always sat on his „tilted“ side, giving him extra support and licking him. It warmed my heart to know that she understood he was unwell and comforted him. Leo eventually made a full recovery.

- It should be offered an unpadded nest where the rabbit can sit comfortably without tipping over. Rolled towels are particularly suitable – the towel rolls are arranged in a C-shape around the rabbit. The rabbit must always have the option to leave the nest. A transport box, for example, works well for this. Food should also be provided there so the rabbit can eat comfortably. If the rabbit has completely lost its orientation and is only squirming/rolling, twitching its eyes, and cannot sit at all, it is best to place it in the transport box and build a small barrier so it doesn’t fall out immediately but can first calm down and rest comfortably.
- The environment must be adjusted to suit the rabbit’s needs. Tunnels provide orientationless rabbits with protection and support. If they tip over, they can get back up on their own. Simply have a board cut into three pieces at a hardware store and screw them together with four brackets to create a tunnel. For active EClers (rabbits with EC), artificially created walls, willow bridges, and wooden tunnels are recommended for orientation.
- The care of paralyzed rabbits is not easy, as they can develop pressure sores (decubitus). The rabbit should be placed on a very soft, wrinkle-free surface (such as bedding with cotton towels on top or disposable changing pads with Vetbeds on top). Vetbeds with wood pellets underneath have also proven to be effective.

- To protect rolling or lying rabbits from eye injuries, it is helpful to place them on clean cotton towels. Additionally, the eye may be temporarily taped shut to prevent injury. However, close monitoring is essential! For paralyzed rabbits, under the guidance of a veterinarian, the downward-facing eye of rabbits that are spinning heavily can be taped shut to protect it from injury. It is important to monitor the eye closely during this time!
- Give hope for life, but only once the rabbit is somewhat stable! For example, you can try to see if a previously outdoor rabbit feels more comfortable outside now and thrives more.

- Once the rabbit is back to being fit, it needs to move a lot (ideally, allow it to roam freely) to retrain its sense of balance and rebuild its muscles. This often results in the head becoming more aligned, and signs of paralysis usually reduce drastically or disappear entirely!
- The medication must be administered gently, without force.
- Provide plenty of fresh food and juices, and possibly also infusions. This can help prevent severe kidney damage, minimize the damage, or allow for regeneration.
- The rabbit should be lifted as little as possible. There are cases where the rabbit needs to be lifted, such as when it becomes heavily soiled and needs a bath, or to bring it to the vet. However, lifting can cause a lot of stress, especially if the rabbit is dizzy and starts rolling as a result. Therefore, each time it needs to be lifted, it should be carefully considered. When setting it down, it’s best to place the rabbit in a padded nest and gently but firmly hold it for a short time until it regains its orientation.
- For active EClers (rabbits with E. Cuniculi), artificially created walls, willow bridges, and wooden tunnels are recommended to help with orientation.

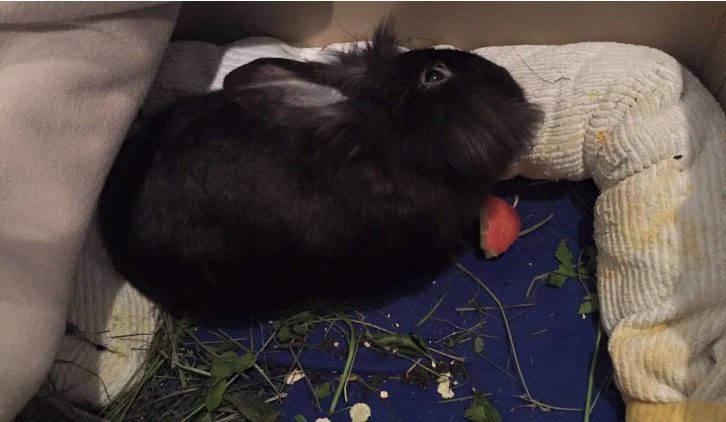
Hand-feeding and food intake
Rabbits with head tilt often have difficulty eating enough food, as they require a lot of energy and can quickly lose weight. During the acute phase, it is important to offer food in such a way that the rabbits can find and eat it, even with a tilted head and disorientation. It is helpful to place the food in various ways and observe how it can be most easily eaten. If the rabbits still eat poorly, kidney insufficiency or another condition (differential diagnoses: pain!) may be the underlying cause.
Rabbits with this condition prefer fresh greens from nature, such as dandelion (also available in Turkish stores), clover, alfalfa, hogweed, plantain, and vegetable greens. For healing, fennel and hogweed are important; these foods can (based on experience) accelerate recovery and are preferred by rabbits with E. Cuniculi. Some herbs have also proven beneficial, including tansy, a small amount of wormwood, mugwort (Artemisia annua), thyme, all types of cress, common ragweed, blueberries, garlic, spring onions, wild garlic, chives, leek, pumpkin seeds, ginger, and many wild, meadow, and kitchen herbs. If food intake is difficult, soaked Cuni Complete can also be hand-fed, which may be helpful.
If the rabbits are only spinning and no longer know which way is up, the food must be placed directly in their mouth, and if necessary, fed with a syringe of mush, which is often eagerly accepted.

Prevention
You can protect your rabbits: the EC status can be determined through a blood test.
Is your rabbit EC-negative?
If a new rabbit is joining your household, it should also be tested negative to prevent it from infecting your rabbits.
Is your rabbit EC-positive?
The pathogen continuously destroys cells in the body, especially during times of stress or illness.
You can prevent acute symptoms by keeping Fenbendazole (Panacur) at home and administering it when:
- Your rabbit is under stress (vet visit, bonding, relocation, etc.) — about 3 days before the event for 5-10 days
- Your rabbit is sick until it recovers
- Your rabbit is to be vaccinated (this makes the vaccination more effective) — about 3 days before the vaccination for 5-10 days
- Your rabbit has a chronic illness (28-day course every 5th month, continuous use if cortisone is given)
- Your rabbit is scheduled for surgery (e.g., neutering) — about 3 days before the surgery for 5-10 days
- For older EC-positive rabbits, kidney values should be regularly monitored to detect kidney diseases early.
- If a new rabbit is joining, choose only EC-positive rabbits to avoid infecting others.

In a study, Panacur was administered for four weeks, and the rabbits were then protected from an outbreak for a little over four months. If Fenbendazole was given recently, a treatment course can be skipped, and there should always be several months between doses.
Disinfection
To minimize spore intake, feeding areas should be kept hygienic, and bowls should be thoroughly cleaned.
Disinfection is only necessary in exceptional cases (e.g., when changing enclosures): E. cuniculi spores are quite resistant to environmental influences. The spores excreted in the environment can be killed by boiling them for five minutes. At room temperature, they survive for about a month; at 4°C, they last over three months; and at 37°C, they survive for two days. The pathogen survives less time in dry cold (less than a week at 4°C).
Some disinfectants are also very effective when spores are exposed to them for 30 minutes: 70% ethanol, 0.3% formaldehyde, 1% hydrogen peroxide, and 1% sodium hydroxide killed 100% of the pathogens. Citric acid killed 81% of the spores, is harmless once rinsed off, and effectively dissolves urine, making it ideal for cleaning wipeable surfaces and toilets.
Case Reports
Henry developed a severe head tilt and the typical spinning in circles within 24 hours. At the vet, he was x-rayed and had blood drawn. Initially, an ear infection (otitis) was suspected, but no changes were observed in the blood. The treatment began with Baytril and Metacam. When no improvement was seen after two days, we did a CT scan to assess the situation more accurately. It was found that there was no ear infection. Blood was then sent for EC testing, and a urine sample was also sent for EC PCR. Both tests came back negative. Despite this, we started a treatment with Panacur. After 7 days of feeding and worrying, improvement was finally seen. Henry started eating on his own again, moving without falling over, and his head became more aligned. Now, four weeks have passed, and he is almost back to normal. The vet mentioned that 4% of rabbits with EC do not form antibodies.


Maja (2 years old)
Maja fell ill with EC in 2021. She couldn’t stand up and rolled around for 8 weeks. I had little hope, but she ate like a little pig, so I couldn’t give up on her. I gave her medication every day, bathed her, placed fresh food in front of her, and so on. The day she sat up for the first time again was beautiful. Now, she has more joy in life than any of my other rabbits. The fight was worth it. Every single day of extra life.


Augustus, about 5 years old
At first, he only had a slight head tilt and refused to eat. Then, day by day, it got worse; he was lying on his side and rolling around. I had to hand-feed him at the beginning. I had to help him with grooming as he was sometimes soiled with feces… Then, suddenly, things started to improve. He kept trying to stand up. It took a total of 6 weeks.


Mats (8 1/2 years old) – approximately 5 weeks until recovery


Mümmeline (8 months old) took about 3-4 weeks to start hopping again. After approximately 8 weeks, she was able to stand on her hind legs again. The veterinarian initially recommended euthanasia. Today, three years later, she is still completely healthy. She is the leader of a group of 9 rabbits.

Tedi with severe E. cuniculi – recovery process: it was only when she was reunited with her partner rabbit (after an initial separation), who cared for her intensively and pampered her, that she slowly began to recover.



Leon, approximately 4 years old, had very poor liver values, a high E. cuniculi titer, a slightly tilted head, and had stopped moving (apathetic). Treatment: Panacur for 28 days, infusions (initially twice daily, then daily, and eventually less frequent), hogweed, and fennel. After three weeks, he was completely healthy again and has not had a relapse since.

Leopold
After 4 weeks of Panacur and additional vitamin B complex, he was back to his old self.

Jaimy (before – after)


Mogli
Before – After
After two months, he was fit again.

Merlin with EC and ear infection
Treatment: 8 weeks of Panacur, two weeks of Baytril, and as long as symptoms persisted, vitamin B complex, Metacam, Vertigoheel, Cerebrum, and Engystol.
X-rays revealed that Merlin also had an ear infection (Note: same symptoms as EC!). Four weeks after the onset, he was given an additional 10 days of Duphamox, followed by two weeks of Marbocyl. During the antibiotic treatment, Pro Pre Bac was administered two hours later to maintain the gut flora. He also received dried meadow hogweed daily and later fresh.
Monica with EC and middle ear infection
Monica is a curious almost 9-year-old lop rabbit, who had never been ill before. Shortly after our vacation, she started to withdraw. At the veterinary clinic, we were told she had bloating. We were given medication and left the clinic feeling relieved. The next day, her head started tilting slightly to one side. We went back to the clinic, as we only noticed this early in the morning. They diagnosed either an ear infection, a brain tumor, or EC, and advised us to treat EC first. When we took Monica to our family veterinarian for a second opinion, she told us we needed to take a strong decision, as the head tilt was too severe. We decided against that and insisted on a CT scan at the clinic. The diagnosis: a unilateral middle ear infection, but the inner ear and bones were not affected. Additionally, the head tilt was in the wrong direction, so the ear infection couldn’t have been the cause.
For the first time, we visited a rabbit-savvy veterinarian. We treated the ear infection with painkillers and antibiotics and continued the EC treatment. First, Monica managed to move without tumbling, then she began grooming herself again, found her way to her pen and the litter box, and 1-2 weeks later, still with a very tilted head, she happily hopped around. Just like before, she explored everything, knocked over tunnels and boxes, and jumped onto various objects. A few days later, her head began to straighten. Currently (about 8 weeks after the onset of illness), she still has a slight head tilt, but it doesn’t affect her at all. We have stopped the Panacur treatment in consultation with our veterinarian. We are trying physiotherapy to relax the shortened muscles, but if her head remains as it is, it wouldn’t be a limitation. In January, we will likely have another CT scan to check how the ear infection has progressed. If necessary, we may have to consider surgery, but thanks to our veterinarian and several success stories, we have many options. It’s worth fighting for, and as difficult as it was at times, it’s now so wonderful to see Monica racing around and jumping again. We hope that our story might give strength to others as well.



Mädi
After weeks of treatment, her head has become completely straight again.


Blacky as a young rabbit, about 3 months old
Shortly after purchasing him from a pet store, EC broke out in Blacky. Overall, Blacky was treated for 3-4 months.



Sources include:
Abu- Akkada, S. S., Oda, S.S. (2016): Prevention and treatment of Encephalitozoon cuniculi infection in immunosuppressed rabbits with fenbendazole. Iran J Vet Res. 17(2): 98–105.
Baneux, P. J. R., & Pognan, F. (2003): In utero transmission of Encephalitozoon cuniculi strain type I in rabbits. Laboratory animals, 37(2), 132-138.
Csokai, J., Joachim, A., Gruber, A., Tichy, A., Pakozdy, A., & Künzel, F. (2009). Diagnostic markers for encephalitozoonosis in pet rabbits. Veterinary parasitology, 163(1), 18-26.
Deplazes, P., Mathis, A., Baumgartner, R., Tanner, I., & Weber, R. (1996): Immunologic and molecular characteristics of Encephalitozoon-like microsporidia isolated from humans and rabbits indicate that Encephalitozoon cuniculi is a zoonotic parasite.
Harcourt-Brown, F. M.; Holloway, H. K. R. (2003): Encephalitozoon cuniculi in pet rabbits
Hein, J., Flock, U., Sauter-Louis, C., & Hartmann, K. (2014): Encephalitozoon cuniculi in rabbits in Germany: prevalence and sensitivity of antibody testing.Veterinary Record: Journal of the British Veterinary Association, 174(14).
Jass, A., Matiasek, K., Henke, J., Küchenhoff, H., Hartmann, K., & Fischer, A. (2008). Analysis of cerebrospinal fluid in healthy rabbits and rabbits with clinically suspected encephalitozoonosis. The Veterinary Record, 162(19), 618-622.
Jeklova, E., Jekl, V., Kovarcik, K., Hauptman, K., Koudela, B., Neumayerova, H., … & Faldyna, M. (2010): Usefulness of detection of specific IgM and IgG antibodies for diagnosis of clinical encephalitozoonosis in pet rabbits.Veterinary parasitology, 170(1), 143-148.
Klang, A., Pakozdy, A., Weissenböck, H., Künzel, F. (2009): A Retrospective Study of Neurological Disease in 118 Rabbits.
Künzel, F., & Fisher, P. G. (2018): Clinical Signs, Diagnosis, and Treatment of Encephalitozoon cuniculi Infection in Rabbits. Veterinary Clinics of North America: Exotic Animal Practice, 21(1), 69–82. doi:10.1016/j.cvex.2017.08.002
Sieg J., Hein J., Jass A., Sauter-Louis C., Hartmann K., Fischer A. (2012): Clinical evaluation of therapeutic success in rabbits with suspected encephalitozoonosis.
Sieg J., Jass A., Fischer A., Hein J. (2010): Vergleich verschiedener Therapiemodelle zur Enzephalitozoonose bei Kaninchen. In: Abstracts der 18. Jahrestag der DVG-FG InnLab 2010.
Künzel F1, Gruber A, Tichy A, Edelhofer R, Nell B, Hassan J, Leschnik M, Thalhammer JG, Joachim A. (2008): Clinical symptoms and diagnosis of encephalitozoonosis in pet rabbits.
Suter C., Müller-Doblies U., Hatt J.-M., Deplazes P. (2001): Prevention and treatment of Encephalitozoon cuniculi infection in rabbits with fenbendazole. Vet Record 2001
Muser RK, Paul JW. (1984): Safety of fenbendazole use in cattle. Mod Vet Pract. 1984 May;65(5):371-4.
Waller, T. (1979): Sensitivity of Encephalitozoon cuniculi to various temperatures, disinfectants and drugs. Laboratory animals 13.3: 227-230.
Ziętek, J., Adaszek, Ł., Dzięgiel, B., Kalinowski, M., Bartnicki, M., Kalinowska, A., … & Winiarczyk, S. (2014). Diagnosis of the Encephalitozoon cuniculi infections in pet rabbits with neurological symptoms. Polish journal of veterinary sciences, 17(2), 361-363.
Dissertationen
Flock, U. (2010): Enzephalitozoonose beim Kaninchen – eine retrospektive Auswertung. Diss. München
Habenbacher, Ch. (2011): Etablierung und Validierung einer Immunhistochemie
und in-situ Hybridisierung zum Nachweis von Encephalitozoon cuniculi, Diss. Wien
Jaß, A. (2004): Evaluierung von Liquorpunktion und PCR zur klinischen Diagnose der Enzephalitozoonose beim Kaninchen. Diss. München
Meyer-Breckwoldt, A. (1996): Epidemiologische und klinische Untersuchungen zur Enzephalitozoonose beim Zwergkaninchen. Diss. Tierärztliche Hochschule Hannover
Neuwirth E. (1988): Enzephalitozoonose. Diss. Tierärztliche Hochschule Hannover
Bücher & Sonstiges
Csokai, J. (2015): Kopfschiefhaltung–Encephalitozoonose? Welche Diagnostikmöglichkeiten gibt es?. veterinär spiegel, 25(02), 72-75.
Fehr, M. (2012): Gefahr durch Encephalitozoonose bei Kaninchen [http://www.tiergesundheit-aktuell.de/videos/kleintiervideo-549.php, 25.4.16]
Felchle L., Sigler R. (2002): Pacoemulsification for the management of Encephalitozoon cuniculi-induced phacoclastic uveitis in a rabbit. Vet Ophthalmol. 5:211–215
Göbel, T. (2002): Die Encephalitozoon cuniculi-Erkrankung beim Heimtierkaninchen. Eine potentielle Zoonose?
Hein, J. (2008): Clinical symptoms and diagnosis of encephalitozoonosis in pet rabbits. [https://www.researchgate.net/publication/5685701_Clinical_symptoms_and_diagnosis_of_Encephalitozoonosis_in_pet_rabbits]
Hein, J. (2008): Enzephalitozoon cuniculi beim Kaninchen – aktuelle Daten DVG-Kongress Düsseldorf 2008 [http://www.kaninchenforum.com/site/images/stories/hein%20dvg%20%20encephalitozoonose%20%28kompr.%29.pdf, 03.04.2010]
Hein, J. (2009): Enzephalitozoonose – retrospektive Auswertung von Patientendaten [http://www.kaninchenforum.com/site/images/stories/abstract%20flock%20hein%20enzephalitozoonose%20innlab%20tp%2002-%2009.pdf, 26.01.2012]
Hein, J. (2012): Achtung Zoonose! Persistierende Infektion mit E.cuniculi [http://www.heimtieraerztin.de/images/docs/ta%20-%20sv_aktuell-enzephalitozoonose.pdf, 01.05.2013]
Künzel, F., Gruber, A., Tichy, A., Edelhofer, R., Nell, B., Hassan, J. & Joachim, A. (2008): Clinical symptoms and diagnosis of encephalitozoonosis in pet rabbits. Veterinary parasitology, 151(2-4), 115-124.
Latney, L. V., Bradley, C. W., Wyre, N. R. (2013): Encephalitozoon cuniculi in pet rabbits: diagnosis and optimal management [https://www.dovepress.com/encephalitozoon-cuniculi-in-pet-rabbits-diagnosis-and-optimal-manageme-peer-reviewed-fulltext-article-VMRR]
Hein, J. (2013): Enzephalitozoonose beim Kaninchen. [http://www.heimtieraerztin.de/images/docs/b%20-%20besitzerinfo%20encephalitozoonose%205-2013.pdf, 13.04.2015]
Hein, J. (2015): Alles Enzephalitozoonose – oder gibt es da noch mehr? Enke Verlag kleintier konkret 2015; 18(S 02): 37–41
Hein, J. (2015):Enzephalitozoonose – immer noch eine Herausforderung in Diagnostik und Therapie. Der Praktische Tierarzt 96, 5(15) [http://www.heimtieraerztin.de/images/docs/Downloads-Tieraerzte/hein-fall%20ec-prkt%20tierarzt%202015-05%20hp.pdf, 13.02.2016]
Jordan, C., Zajac,A. M., Lindsay, D. S. (2006): Encephalitozoon cuniculi Infection in Rabbits.
Khan, I. A., Moretto, M., & Weiss, L. M. (2001): Immune response to Encephalitozoon cuniculi infection. Microbes and infection, 3(5), 401-405
Künzel, F., Joachim, A. (2010): Encephalitozoonosis in rabbits. Parasitology research 106.2 : 299-309.
Rosenthal, K. L. (2004): Therapeutic contraindications in exotic pets. In Seminars in Avian and Exotic Pet Medicine (Vol. 13, No. 1, pp. 44-48). WB Saunders.
Meredith, A., & Lord, B. (2014). BSAVA manual of rabbit medicine. British Small Animal Veterinary Association.
Meredith, A. L., Richardson, J. (2015): Neurological Diseases of Rabbits and Rodents.
Meyer-Breckwoldt A. (1996): Epidemiologische und klinische Untersuchungen zur Enzephalitozoonose beim Zwergkaninchen. Diss med vet, Hannover
Oglesbee, B. (2011): Blackwell´s Five-Minute Veterinary Consult: Small Mammal, 2nd Edition
Ozkan, O., Ozkan, A. T., & Zafer, K. (2011): Encephalitozoonosis in New Zealand rabbits and potential transmission risk. Veterinary Parasitology, 179(1-3), 234-237.
Sandmeyer, Lynne S., Bianca S. Bauer, Bruce H. Grahn (2011): Diagnostic Ophthalmology. The Canadian Veterinary Journal 52.9: 1023.
Varga, M. (2014): Textbook of Rabbit Medicine. Second Edition.




















