Jaw abscesses are unfortunately a common condition in rabbits. Treatment is quite complex, but when carried out correctly, rabbit-savvy dental veterinarians can often cure the abscesses.
Contents
Symptoms
Usually, only one or two of the listed symptoms appear.
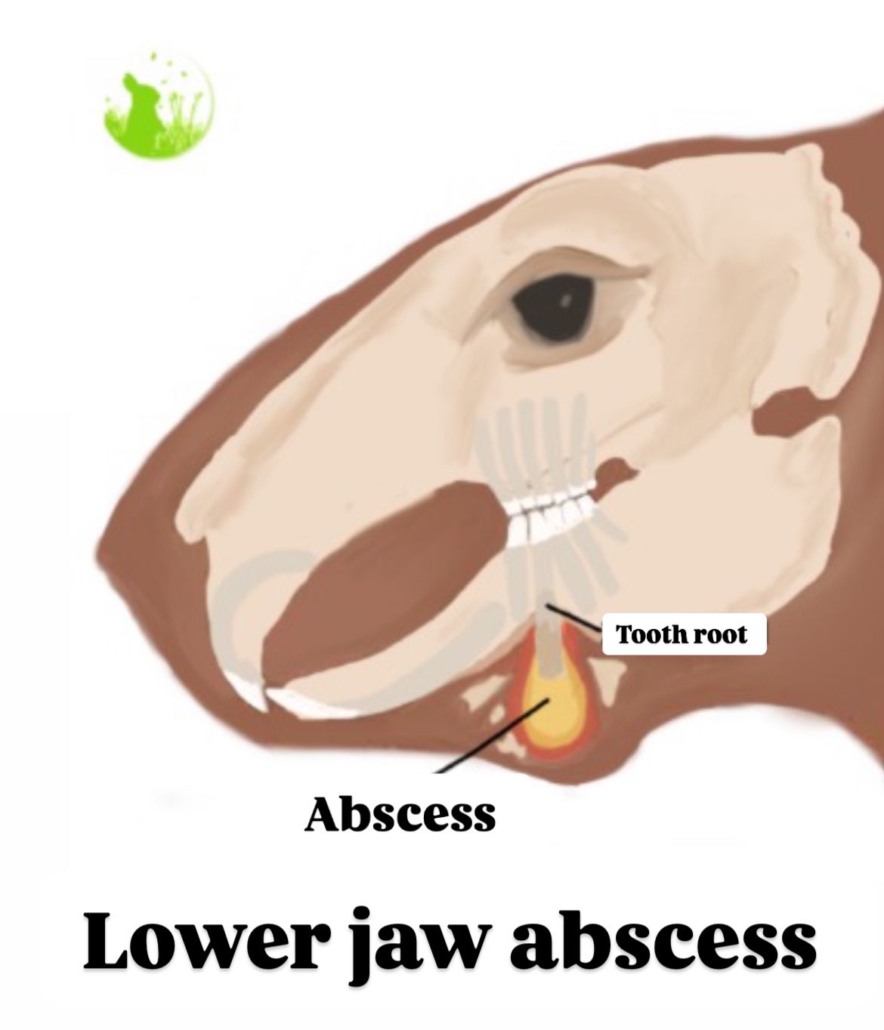
- Abscesses in the lower jaw are often easy to feel or see (swelling/thickening).
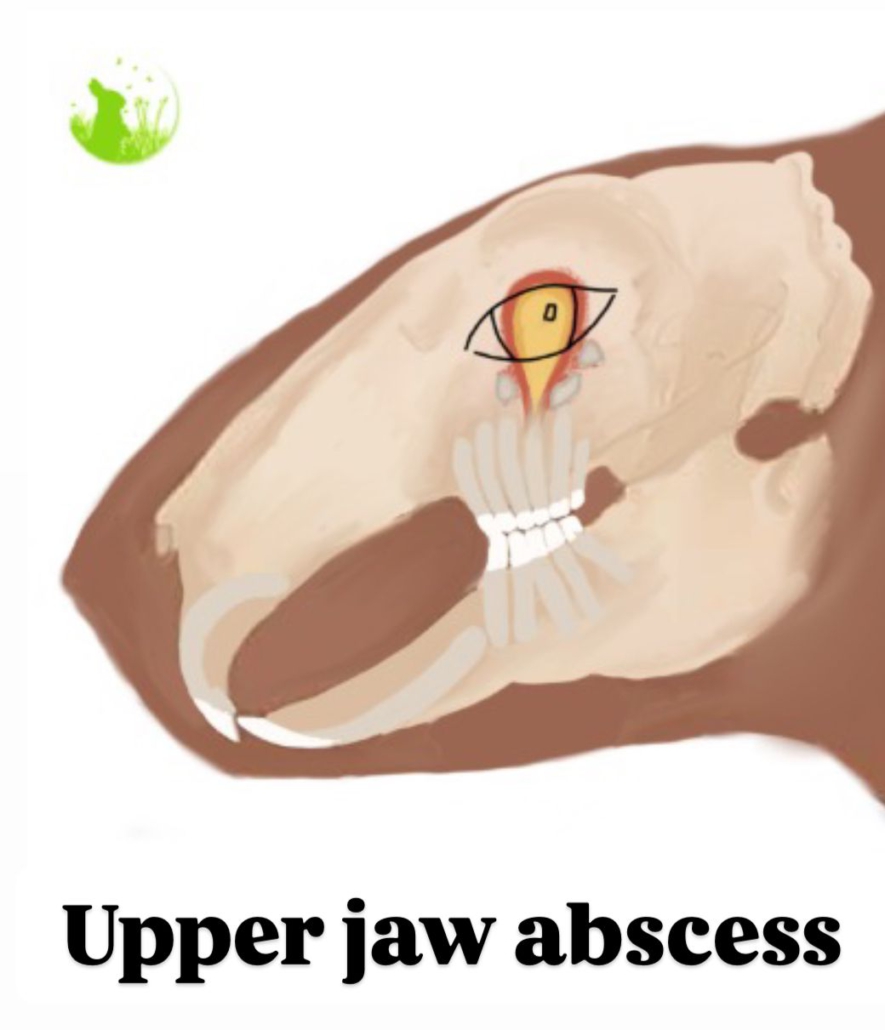
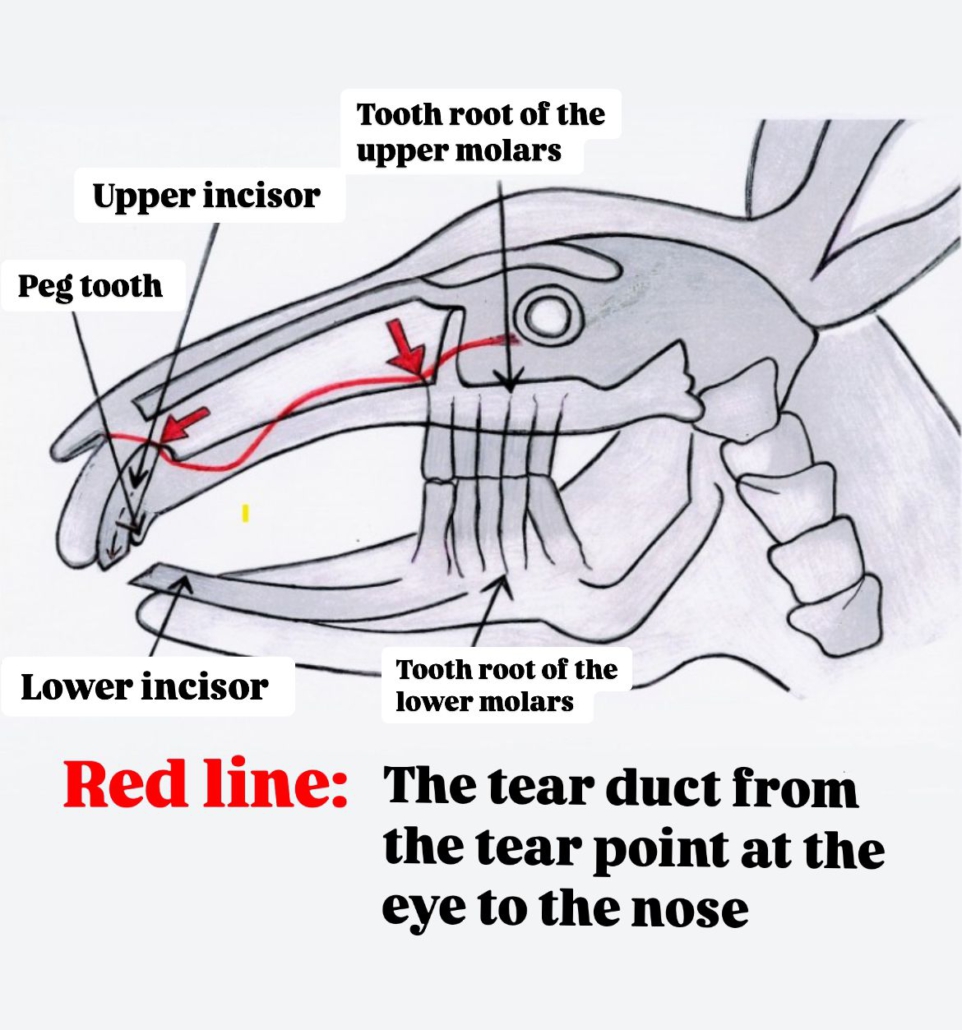
- Abscesses in the upper jaw often present with purulent nasal discharge or normal eye discharge (due to the abscess breaking into the nasal cavity) or ear infections (which often go unnoticed). In some cases, the eye may bulge slightly, leading to facial asymmetry. Mild breathing problems can also occur if the nose becomes clogged with pus.
- Some rabbits selectively eat soft food, eat less than before, or stop eating entirely.
In many cases, the veterinarian may have noticed uneven tooth wear, as the rabbit chewed primarily on one side to avoid pain on the affected side.
Some rabbits may drool (resulting in a wet chin).










Causes
The most common cause of jaw abscesses is an infection of the tooth roots, which can be triggered by:
- Dental diseases: These are often caused when teeth are trimmed with pliers by a veterinarian, leading to microfractures that can result in infected tooth roots. For dental issues, ensure that teeth are exclusively filed or trimmed using rotary tools, never clipped.
- Chewing on foreign objects (e.g., small stones in pellets).
- Misalignments due to genetics (poor breeding practices).
- Inappropriate diet: For example, retrograde tooth growth caused by feeding pellets or loose teeth.

Or through an infection in the subcutaneous tissue, which is often triggered by:
- Injuries caused by sharp tooth edges (resulting from dental disease due to insufficient tooth wear).
- Sharp objects.
- Bite wounds (from dominance fights, etc.).
- Foreign objects in the food.
Rabbits with dental diseases may get thorns or other food particles stuck between their teeth, which are harmless for healthy rabbits.
Many aerobic and anaerobic bacteria can be considered potential causes of abscesses. Various pathogens have been identified, including Pasteurella, Staphylococcus, Pseudomonas, Pasteurella multocida, and Escherichia coli.
Infections caused by dental disease or foreign objects can lead to the production of pus. Because rabbits absorb the liquid from the pus, a thick, sticky white pus forms that does not easily drain when the abscess is opened. This is why rabbit abscesses are particularly persistent.
Many abscesses grow very slowly and go unnoticed, as they are not necessarily painful in the early stages. However, the pus progressively spreads, and since jaw abscesses are located in the head, they often reach regions critical for vital functions. This can lead to ear infections, nerve involvement, respiratory issues, or even infection of the jawbone.
Diagnosis
In addition to jaw abscesses, tumors or bone cysts are also possible causes of facial swelling.
The diagnosis depends on the location of the abscess and involves the following methods:
- Thorough palpation of the head and abscess: Checking if it is well-defined.
- Examination of the oral cavity: Looking for discolored or loose teeth, and observing if pus is discharged when pressure is applied to the abscess.
- Aspiration with a needle: To check if pus is present.
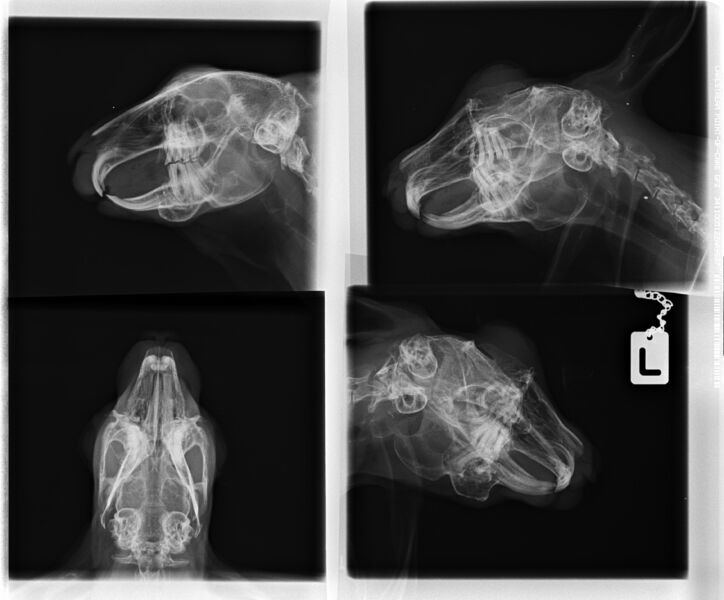
- Head X-rays: Taken from multiple angles, with particularly well-positioned lateral and dorsoventral views.
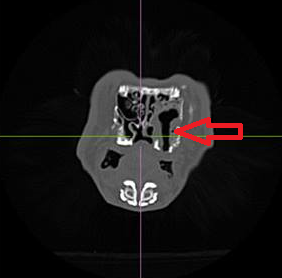
- Computed tomography (CT) or magnetic resonance imaging (MRI): These are used to determine the extent of the abscess, assess treatment prospects, identify the most effective treatment method, and clarify the underlying cause (e.g., dental disease and which teeth need to be removed).
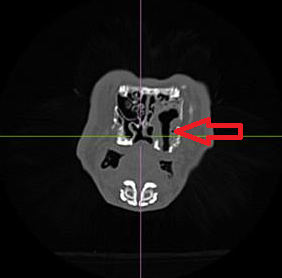
If your rabbit has purulent or unilateral nasal discharge, or if there is swelling in the jaw area, your veterinarian should independently recommend X-rays from at least two different positions (minimum of 2, preferably 4 views), or other imaging diagnostics (MRI, CT). If this is not the case, you should definitely switch to a rabbit-savvy dental veterinarian!
Only with proper diagnostics can the treatment be carried out successfully. Through imaging diagnostics, the veterinarian can determine which teeth are the cause of the issue, how extensive the abscess is, whether it has already led to an infection in the middle and inner ears, and how much the jawbone is affected. Without imaging diagnostics, no veterinarian can provide these details!
Unfortunately, there are still veterinarians who do not perform X-rays and treat the abscess without determining its exact extent, cause, and potential complications. As a result, cases arise that require months of costly treatment, yet the abscess keeps recurring. These animals often have to be euthanized after a long period of suffering. This could have been avoided with simple diagnostics and expert treatment from the outset.

Treatment
Prognosis
The chances of success depend on several factors:
- Veterinarian’s Expertise: How knowledgeable and specialized is the veterinarian in rabbit dentistry? An experienced vet with specialization in rabbit dental issues can significantly impact the success of the treatment.
- Location of the Abscess: Where exactly is the abscess located? Some areas are harder to reach than others. In the lower jaw, the abscess cavity is more exposed to contamination from food than in the upper jaw.
- Condition of the Rabbit’s Teeth: How are the remaining teeth of the rabbit? Are they healthy, or does the rabbit have severe dental misalignment? If the abscess affects one side of the jaw and the other side is intact, the rabbit may still be able to chew after surgery. However, it’s important to note that even without an intact chewing surface, most rabbits can adapt and live well with this limitation.
- Number of Affected Teeth: How many teeth are affected by the abscess? The more teeth that are involved, the more complex the treatment may be.
- Bone Involvement: Is the bone affected or resorbed? Where and to what extent is the bone involved? Advanced bone damage can affect the prognosis.
- Surgical Technique: Was all the infected tissue removed, and was the underlying cause (e.g., affected teeth) addressed? Were the affected teeth extracted and the abscess fully treated?
- Is the owner willing to allow all necessary procedures and follow-up care?
- Rabbit’s Temperament: How does the rabbit respond to the treatment? Does it start eating quickly again, and is it willing to take the required medications? An active and cooperative rabbit has a better chance of a successful recovery.
- Postoperative Care: Is the rabbit receiving intensive care after surgery? Is it being hand-fed, receiving the proper medications, and offered appealing food to encourage eating? Is the owner willing to administer the necessary antibiotics, possibly by injection?
These factors together determine the prognosis and success of treating an abscess in rabbits. Early diagnosis and proper treatment are crucial for the best possible healing and the animal’s quality of life.
Treatment Options
Conservative Treatment with Antibiotics and Painkillers (without Surgery): This is only useful in rare cases when the rabbit is eating well and the jaw abscess has a real chance of healing (for example, when no teeth or other causes are found). In most cases, however, the pus continues to spread, and the animal may ultimately need to be euthanized. Only in rare cases does the abscess shrink and encapsulate itself. This treatment is often used in older rabbits who would not survive surgery or when owners do not have access to an experienced surgeon nearby.

Surgical Treatment: For this type of treatment, it is beneficial to have an experienced veterinarian with strong dental and surgical skills. The abscess cavity is opened, and the thick, viscous pus is scooped out or flushed. During a thorough examination of the abscess, any involved teeth may be extracted or foreign bodies removed. All infected tissue and, if possible, the entire abscess capsule should also be removed. The wound area will then be treated intensively. Normally, the access to the abscess cavity should remain open after surgery, allowing for continued monitoring or treatment, although in some cases the abscess may also be closed.
Complications/Consequences: Bleeding/blood loss, contamination through the opening to the mouth (where the tooth was extracted), jaw fractures in already damaged bones, recurrence of the abscess, insufficient wear of the opposing teeth (not a concern with a single tooth removal), anesthesia complications.
Postoperative Care: Ensuring proper care after surgery is essential (see below).
Which Antibiotics?
Choosing the right antibiotic is crucial when treating jaw abscesses. For rabbits, only the active ingredients Enrofloxacin and the sulfonamides Sulfadimethoxin (Relardon®) and Sulfaquinoxaline are approved. Therefore, other antibiotics must be repurposed for treatment. Studies on rabbits with jaw abscesses show that bacterial colonization can vary greatly, with involved bacteria coming from both the aerobic and anaerobic environments. For this reason, it is recommended to perform a microbiological examination with an antibiogram. The sample for the antibiogram is not taken from the pus, as it usually only contains non-replicating pathogens, but from the surrounding areas that bleed when scraped. Often, (existing) anaerobes are not detectable but should always be covered by antibiotics. The creation of the antibiogram usually takes about a week, during which time the rabbit must already be treated with antibiotics.

For this period, suitable antibiotics include:
- Chloramphenicol,
- Tetracyclines, or
- A combination of fluoroquinolones and metronidazole.
Suitable antibiotics for the treatment of jaw abscesses:
Based on the antibiogram, but always cover anaerobes as well!
Fluoroquinolones (Enrofloxacin, Marbofloxacin, Ciprofloxacin), e.g., Baytril (10 mg/kg twice daily), Marbofloxacin, e.g., Marbocyl (10 mg/kg once daily), always in combination with Chloramphenicol, Amoxicillin, Tetracycline, Pradofloxacin, or Metronidazole.
Chloramphenicol (20–40 mg/kg twice daily) shows very good effectiveness against anaerobes and often has an effect against aerobes as well. It is well-tolerated, even when administered orally.
Tetracyclines are very effective against anaerobes and have average effectiveness against aerobes. They are also well-tolerated.
Penicillins (never orally, only injected): e.g., Amoxicillin, Streptomycin (usually Duphamox, 10–20 mg/kg once daily or Veracin RS 0.1 ml/kg once daily). Amoxicillin is very effective against anaerobes and average against aerobes. Amoxicillin can lead to fatalities and digestive issues, so it should only be used after strict indication and when the digestive system is functioning well.
Metronidazole (25 mg/kg twice daily or 40 mg/kg twice daily orally) is effective against anaerobes (except Actinomycetes) and is very well-tolerated. If there is also an infection with aerobes, it can be combined with fluoroquinolones.
Trimethoprim/Sulfadiazine, e.g., Cotrim K (40 mg/kg twice daily), has good effectiveness against both aerobes and anaerobes.
Sulfonamides are unsuitable as they work well against aerobes and are well-tolerated but do not work against anaerobes. As a bacteriostatic antibiotic, they cannot be combined with other active ingredients!
Gentamicin is recommended only for local use (e.g., in the mouth) if it is sensitive in the antibiogram, as systemic administration can harm the kidneys.
Supportive Treatments and Care
- When treating jaw abscesses, it is crucial to offer a large amount of food around the clock. This should include a variety of tasty greens (e.g., endive, carrot greens, kohlrabi leaves, clover, dandelion…) as well as food that requires little chewing (e.g., soaked Cuni Complete from pet stores).
- Medications must be administered reliably. The owner should be willing to learn how to administer injections, as highly effective antibiotics, such as penicillins, can be used when necessary. The animal will need high doses of pain relief (Note: for rabbits, these are often dosed higher than for dogs and cats!), typically a combination of multiple pain medications, to stimulate eating. You can learn how to gently administer medications here.
- Ensure that all necessary surgeries are performed. Consult a specialized veterinarian and have the abscess properly diagnosed (e.g., head X-rays from four different positions, CT, or MRI!).
- Postoperative Care: Provide a calm environment, intensive care with supplementary feeding of soft food, and adequate pain relief and antibiotic administration. A wide range of food options should be offered, including the rabbit’s favorite foods, enticing leafy greens (e.g., carrot greens, dandelion, kohlrabi leaves, clover, alfalfa, grass…), soaked dry food (e.g., Cuni Complete).

- Mucolytics such as Acetylcysteine (ACC) and Bromhexine can help liquefy the pus, often improving the effectiveness of antibiotics.
- The rabbit can be supported with anti-inflammatory foods such as radish, horseradish, nasturtium, ginger, and cress. Since these foods may have poor acceptance, they can be mixed with the rabbit’s favorite foods.
- If the abscess is not properly diagnosed and surgically treated, it will continue to spread in the head area. Rabbits often do not show signs of pain, so the owner may not realize that the condition is worsening. However, if only antibiotics are used without surgery, the treatment success must be closely monitored with radiographic diagnostics to ensure the rabbit is not suffering.
- Depending on the condition, some teeth may need to be removed. Depending on which teeth are removed, the food will need to be adjusted to the dental situation (e.g., soaked dry food, grated vegetables, finely chopped food…). More information is available here.







Case Reports
Moritz, a satin rabbit with many jaw abscesses and dental problems
His entire lower right row of teeth and one lower incisor were removed. Through surgeries and long-term antibiotics (Amoxicillin), it was possible to get it under control, allowing him to live for several more years without abscesses.







Mia
Mia had severe abscesses in two quadrants and generally very bad teeth. In several surgeries, all of her molars were removed (first the abscesses on the upper right and lower left, then gradually depending on the severity). She still has all of her incisors. One of the front teeth was also affected at the root by the inflamed molars, but it grew back healthily after the diseased molars were removed. She now eats Cuni Complete from the feeder (two handfuls daily) and vegetables (cucumber, cabbage, bell peppers, etc.—soft foods that she can bite into, no more grass), and you wouldn’t notice that she no longer has molars. Even though the thought of a rabbit without teeth initially seemed strange to me, I would say I would do it again. She became ill at 3 years old and is now 10 years old, and after her dental treatment was completed, she no longer had to visit the vet for her teeth and is completely healthy!



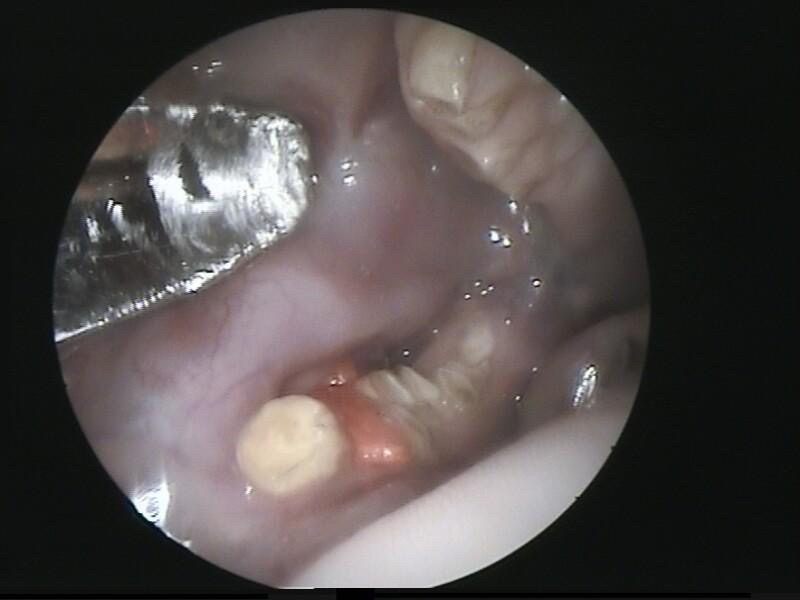
Upper jaw abscess with surgery, drainage, and intensive aftercare and nursing over 3 weeks.


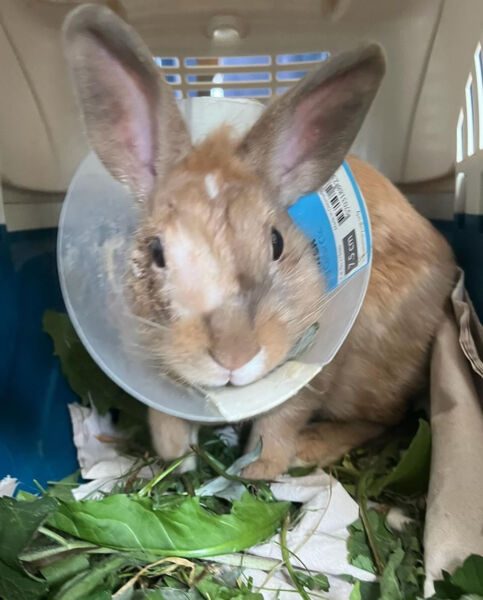



Note: For rabbits, a cone should be replaced with a soft fabric version, or, in many cases, it is unnecessary and can be omitted entirely.
Bruno
Bruno had nasal discharge (purulent) and was initially misdiagnosed and mistreated for rabbit snuffles. A CT scan revealed a severe upper jaw abscess, and his entire upper row of teeth was removed in two surgeries. As a result, the opposing teeth in the lower jaw were no longer worn down naturally and initially had to be trimmed every three months, later only annually (they grow more slowly without counterpressure or stop growing altogether). Unfortunately, due to a treatment error, complications arose, resulting in an oronasal fistula (a connection between the nose and mouth), causing food to occasionally get into his nose and be sneezed out. Despite this, he lived a happy and active life until the age of 10 and ultimately passed away from a tumor in his intestine.


Minnie with Jaw Abscess
A rabbit with very severe dental issues („end-stage teeth“). Minnie was already receiving monthly dental treatments when the swollen cheek caused by a tooth abscess appeared, which was then surgically treated. As bad as such photos may look, things do get better, and Minnie is doing great today.








Sepperl



Sources/Further Reading:
Ewringmann, A. (2016): Leitsymptome beim Kaninchen: diagnostischer Leitfaden und Therapie. Georg Thieme Verlag.
Ewringmann, A. (2017). Keimspektrum und Antibiotikasensitivitäten bei eitrigen Zahnerkrankungen von Kaninchen. Tierärztliche Praxis Kleintiere/Heimtiere, 45(06), 373-383.
Gabriel, S. (2016): Molarenextraktion bei Heimtieren–Indikation und Technik. kleintier konkret, 19(S 02), 18-22.
Gabriel S. (2016): Praxisbuch Zahnmedizin beim Heimtier. Stuttgart: Enke
Glöckner, B. (2002): Untersuchungen zur Ätiologie und Behandlung von Zahn-und Kiefererkrankungen beim Heimtierkaninchen (Doctoral dissertation, Freie Universität Berlin, Universitätsbibliothek).
Göbel, T., & Macha, M. (2008): Dosierungstabellen für Nagetiere und Kaninchen. kleintier konkret, 11(03), 22-27.
Harcout-Brown, F. (2009). Dental disease in pet rabbits 3. Jaw abscesses. In practice, 31(10), 496-505.
Hartmann, M. (2007): Zahnextraktion hypsodonter Zähne bei Nagern und Hasenartigen. veterinär spiegel, 17(01), 22-27.
Kraft, W., Emmerich, I. U., & Hein, J. (2012): Dosierungsvorschläge für Arzneimittel bei Kleinnagern, Kaninchen und Frettchen. Schattauer Verlag.
Medirabbit: Sichere Antibiotika für Kaninchen. [http://www.medirabbit.com/GE/Safe_medication/Antibiotics/sichere_antibio_ge.htm, 8.12.17]




















